Above one of the many carry bags from Sugar Medical Diabetes Accessories. This post was written by Carolyn Jäger, President of the company, whose fun, fashionable bags and accessories make living with diabetes a little easier – and a lot more organized.
Carolyn: “While I got type 1 diabetes at 13, it was when a friend was having a pancreas transplant, that I turned my once childhood insecurities into a company.
I was diagnosed with type 1 diabetes (T1D) at age 13, but I had been living in a household with T1D since I was eight, when my sister was diagnosed. My family was familiar with all the needles (and tears) and glucose monitors, which only made the news of my diagnosis more devastating. I knew enough to be scared and upset that I too would now have to give myself shots for the rest of my life.
Particularly, I hated carrying all my diabetes supplies in “that black medical bag” that comes with every glucometer. It made me stand out but NOT in the way a 13-year-old wants. I carried that bag with me every day, and everywhere – going to the nurse’s office to check my blood sugar, to sports practice, to a friends’ house – and I kept it hidden. It seriously clashed with my 13-year-old fashionista style! (Well, at least I thought I had style back then.) More than anything, I wanted to fit in. Forget it! I began to resent having type 1 diabetes.
Sensing my insecurity, my mother handmade a special bag for my supplies. It was stylish; it had pink fabric and green turtle patches sewn on it. The bag not only suited my presumed sassy style, but it made my life easier. The bag grew my confidence, I even grew comfortable enough to check my blood sugar in front of other people. My mother’s gift also started something I would continue: through the years I sewed my own fun diabetes supply bags for myself.
Then, after I had my first son, a close family friend who had serious complications from diabetes had a pancreas transplant. It rattled and changed me. I became over diligent about testing and tried to prevent myself from ever having a high blood sugar. I constantly corrected my insulin pump in fear of what complications could someday come my way.
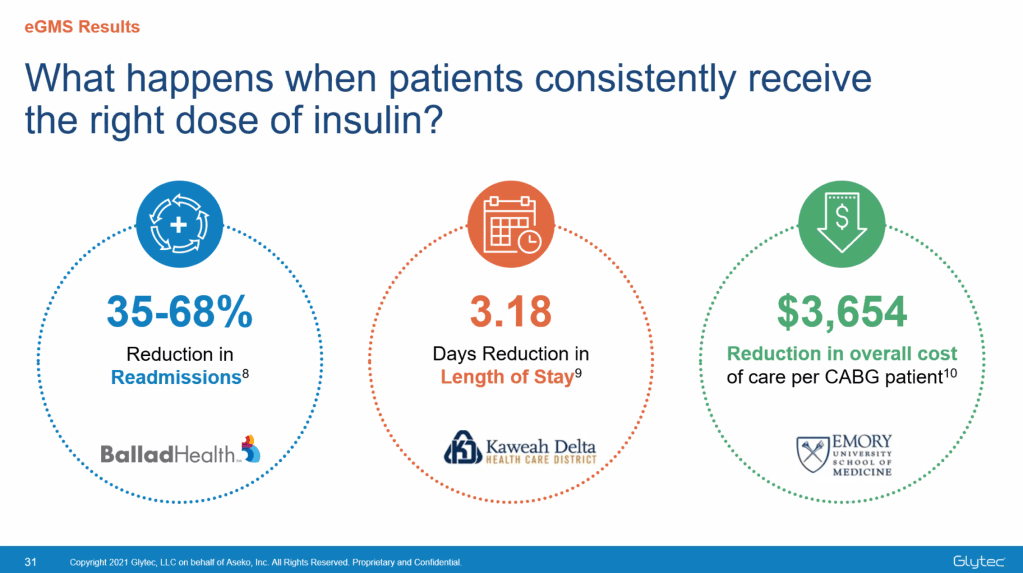
I knew how important good glucose was in controlling diabetes and in preventing complications, and I fiercely wanted to encourage others to check their blood sugar more often. I never wanted to see anyone else suffer as my friend had.
When I shared my desire with my doctor, he explained that many people put themselves at risk because they don’t carry their supplies with them. They feel it’s “too hard to carry everything” or they’re embarrassed by the “medical” looking bag. I realized I wasn’t the only person with diabetes who felt self-conscious about carrying “that black nylon bag!” So I couldn’t be the only person who wanted something better than what was offered free with every glucose meter.
That’s when it dawned on me that I could help others take better care of themselves. I could encourage them to have their supplies close at hand by doing what I did growing up: create a line of bags that look the opposite of “medical” bags, that are fun, stylish and functional. And that’s how Sugar Medical began. Having had a career in retail, and as a buyer for a department store, it turned out I had good training to launch this company, in addition to my childhood bag making career.
Today, 32 years after my diagnosis, I am much more confident about living with type 1 diabetes. I grew to understand that I do not need to hide my illness from others: it is a part of me. I wear my pump proudly on my hip and I have no problem checking my blood sugar in front of people.
I wish I had been this confident as a teenager, but if I had, Sugar Medical probably never would have happened, and I’m glad it did. I, and all who work with me, want to make life a little easier for those of us who live with type 1 diabetes. I won’t be embarrassed to say, take a look at our bags and see if one doesn’t seem perfect for you. It just may be your inspiration to take your management to the next level.”

Our Mission
Sugar Medical encourages more frequent blood glucose checking with diabetes supply bags you will not feel embarrassed to carry – or show off! Sugar Medical gives back to the diabetes community donating yearly to the JDRF, Beyond Type 1 and the College Diabetes Network. We also participate in the walks and events hosted by the JDRF and ADA and support our own community in Midlothian, VA: last year we donated $1.5K to Chesterfield County Food Bank and plan to continue to support this charity.