
I would say I’m late to the game but honestly I haven’t seen much discussion about Dexcom’s relatively new G7 CGM. I actually received my initial order back in mid-March, but waited til a week ago to try on my first, as I wanted to use up my G6 sensors and transmitter first.
Given the title here you know I’m not loving this new version, but before I get to my negatives, I’ll tell you what I do like based on just a week of wear.
What I like
Half hour or less to warm up. Yup, it’s fast and that feels terrific, no more endless two hour wait. The reason it’s typically less than even 30 minutes is by time you’ve gone through the few insertion steps, you’ve shaved a few minutes off.
Sensor and transmitter in one piece. Yes, I do like this. No more extra step to stick the transmitter into the sensor cradle or worry I’ll lose it somehow.
12 hour grace period. I haven’t used this feature but I know you get 10 days and 12 hours out of the G7. Presumably the extra 12 hours is to make it convenient for you whenever you change your sensor.
What I don’t like
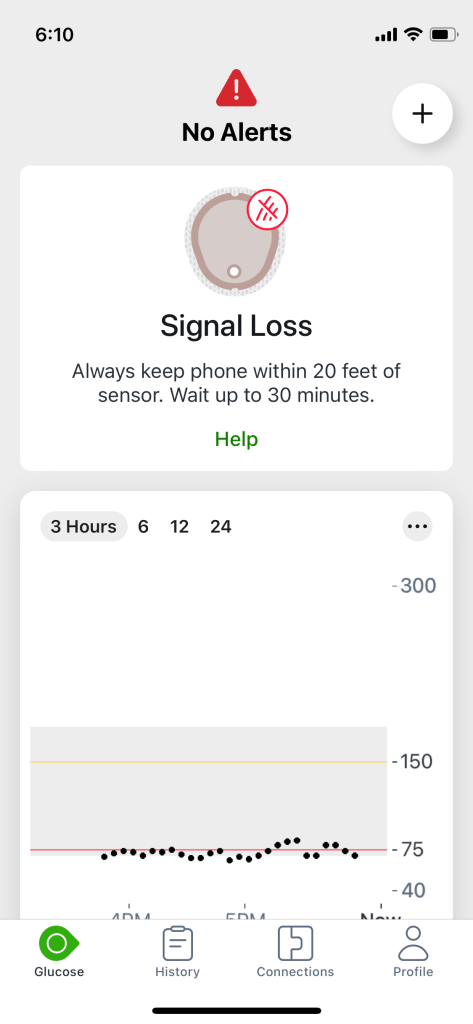
The signal gets dropped multiple times a day. The G7 has the same range as the G6, 20 feet. Yet half the time I look for my number (I use it on my iPhone, I didn’t get a receiver through Medicare, and wouldn’t use it anyway), there’s no signal and I have to wait a few minutes for it to show up. And I know I’m never out of range, I can’t be further away from my phone than 20 feet in my small apartment. This lost signal ‘feature’ is as annoying as the 30 minute warm up time is great.
No widget. With the G6 I never had to open my iPhone to see my numbers. No such luck with the G7, I have to go into my phone, what a pain, to pull it up.
First day numbers. Terrible, inaccurate. With the G6, half the time the sensor worked right out of the box, the other half my first 6-8 hours were spot on with the next 16 wonky. With the G7, the first 24 hours are wonky.
The interface. The G6 range graph was relatively attractive, as attractive as one of these can be. The zones were demarcated in pink, grey and yellow. This face is simply black, white and grey. Devoid of color I find it more clinical and less friendly.
The inserter. No I don’t like it any better than the G6 inserter. In fact, the very first sensor I inserted caused me to bleed and I wore it for two painful days and it never got accurate so, of course, I changed it out. While my second insertion went fine, I experience the insertion as a bullet’s impact (not that I’d know) but definitely too powerful.
The overpatch. Each sensor comes with its own overpatch. There’s so little adhesive around the sensor Dexcom gives you an overpatch, which they instruct you to put on immediately. For me, the smaller size of the sensor is all but ruined by this big piece of white tape running around it. I hate it. I ruined the second overpatch as it stuck to my fingers, so I hauled out the old sheer tape I used to tape the G5 down with, which made me wonder: why couldn’t they at least have made the overpatch clear?
The app. It’s spared down, nothing seems to be shelved where I’d expect to find it, and not user friendly.
In conclusion, the smaller size and rounder shape don’t mean enough to me to compensate for the things I don’t like. The MARD, which means how accurate it is, is slightly better than G6 but, for me, unnoticeable. There’s a feeling Dexcom rushed this one out of the gate and I wonder how many PWDs they consulted with. I can’t imagine a lot of these hiccups would exist if they’d listened to users.
Compared to the Freestyle Libre 3, I think Dexcom has reason to worry. When Libre finishes jumping through the FDA’s hoops, which will likely be this year, and is Medicare covered, I’d absolutely consider switching. Libre is still smaller and thinner than the G7, yes it has one hour warm up time but 14 day wear as compared to Dexcom’s 10, I find it a better inserter, I didn’t experience a dropped signal when I wore the Libre 3 as a courtesy for six weeks, and its accuracy is just about the same.
If you’ve tried the G7, I’d be curious what you think. If you want to see the G7 in action, have a look.